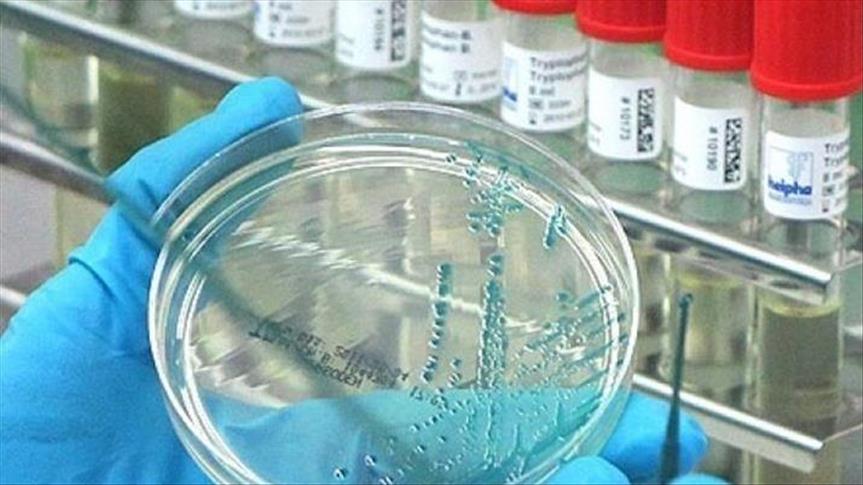
Thirteen individuals have become ill from a serious and
sometimes fatal fungal infection previously unseen in the United
States, the Centers for Disease Control and Prevention said Friday.
The fungus, Candida auris, is known to occur in health care
settings such as hospitals and nursing homes.
Seven cases occurred between May 2013 and August 2016 in four
states: Illinois, Maryland, New Jersey and New York. As of August
31, four of these seven patients, all with bloodstream infections,
died, though it is unclear whether their deaths were due to C.
auris.
The remaining six cases were identified after August and are
still under investigation.
"It appears that C. auris arrived in the United States only in
the past few years," Dr. Tom Chiller, chief of the CDC's Mycotic
Diseases Branch, said in statement. He added that scientists are
working to better understand the fungus so they can develop
recommendations to protect those at risk.
C. auris bloodstream infections have a 50% fatality rate in some
countries, according to one study. Some strains of this yeast are
multidrug-resistant and cannot be treated by the three major
classes of antifungal medications. First reported in 2009 in Japan,
cases have been recorded in South Korea, India, South Africa,
Kuwait, Colombia, Venezuela, Pakistan and the United Kingdom.
"Experience outside the United States suggests that C. auris has
high potential to cause outbreaks in healthcare facilities," the
CDC notes on its website. Importantly, this deadly organism is
difficult to identify using traditional laboratory biochemical
methods.
In response to international reports, the CDC issued an alert in
June to see whether C. auris might be present in the United States.
After hospital and other health care facilities across the nation
performed investigations, the CDC discovered 13 cases had occurred
in the US over the past few years.
A CDC report published Friday describes in detail the first
seven US cases reported to the CDC as of August 31, 2016, in four
states: Illinois (2), Maryland (1), New Jersey (1) and New York
(3).
Laboratory evidence suggests that these seven US cases are
related to those in South America and South Asia, with transmission
occurring within the health care settings, according to the CDC.
Nearly three-quarters of the C. auris strains in US patients showed
some drug resistance, but none was resistant to all three
antifungal drug classes.
All patients had serious underlying medical conditions,
including tumors, vascular disease and bone marrow transplants. The
average time from hospital admission to isolation of C. auris was
18 days. Five patients with bloodstream infections had central
venous catheters at the time C. auris was identified.
Weeks to months after the initial infection, patients had C.
auris on their skin and other areas of the body; according to the
CDC, this could present opportunities for contamination of the
health care environment. Additionally, samples taken from multiple
surfaces in one patient's hospital environment showed contamination
of C. auris.
CDC Director Dr. Tom Frieden called the fungus an emerging
threat and said, "We need to act now to better understand, contain
and stop the spread of this drug-resistant fungus."
In announcing these cases, the CDC reminded health care
facilities of the need to follow cleaning and disinfection
protocols to control and prevent the spread of all fungal
infections.
In 2011, there were 722,000 health care-acquired infections in
US acute care hospitals, according to the CDC, and about 75,000
patients with these infections died during hospitalization.